Editor’s NoteWelcome to the most recent issue of Innovations in Oncology Management™, a newsletter series providing up-to-date information on current issues that are directly affecting the management and business of cancer care in the community. This fifth newsletter in the second series has been developed for oncology practice administrators, administrative staff, advanced practice clinicians, and oncology pharmacists. The current newsletter focuses on the ongoing implementation of Meaningful Use legislation for health information technology and electronic health records. Changes to the federal program were announced in October 2015. These changes affect not only Stages 1 and 2, which are already in progress, but will also impact Stage 3, which is slated for implementation beginning in 2017. With Stage 3 looming on the horizon and incentives shifting to penalties for oncology providers who do not demonstrate proficiency in Meaningful Use, it is vital for oncology practices to redouble their efforts to comply with the federal mandates. We hope that you find this newsletter to be a valuable resource for your practice. Previous newsletters have explored a variety of topics related to oncology practice administration and can be found at www.innovationsinoncologymanagement.com. |
The American Recovery and Reinvestment Act, enacted in 2009, established incentive payments to physicians, hospitals, and Medicare Advantage plans to promote the adoption and meaningful use of health information technology and electronic health records (EHRs). According to the Centers for Medicare & Medicaid Services (CMS), the term “meaningful use” refers to the utilization of certified EHR technology to1,2:
- Improve quality, safety, and efficiency, and reduce health disparities
- Engage patients and families in their care
- Improve care coordination, and population and public health
- Maintain privacy and security of patient health information.
The legislation sets specific objectives that eligible professionals and hospitals must achieve to qualify for incentive payments.1,2
The Meaningful Use legislation is being implemented in 3 stages over a period of several years2: - Stage 1, implemented beginning in 2011, established requirements for electronically capturing clinical data, including providing patients with electronic copies of health information
- Stage 2, implemented beginning in 2014, expanded upon the Stage 1 criteria, encouraging the use of health information technology for continuous quality improvement at the point of care and the exchange of information in the most structured format possible
- Stage 3, which will be implemented beginning in 2017, will focus on enhancing health information exchange functionality, while maintaining an emphasis on continuous quality improvement.
EHR Incentive Programs
As part of the Meaningful Use legislation, CMS is authorized to provide incentive payments to eligible providers that meet the new standards. The Medicare and Medicaid EHR Incentive Programs apply to all eligible professionals and hospitals that treat patients with Medicare (fee-for-service or Medicare Advantage) or Medicaid patients. Under the program, CMS provides EHR incentive payments to physicians or hospitals as they adopt, implement, upgrade, or demonstrate meaningful use of certified EHR technology.3
Eligible professionals can qualify for EHR incentive payments totaling as high as $44,000 through the Medicare EHR Incentive Program. Similarly, eligible hospitals can qualify for EHR incentive payments of $2 million or higher. The Medicare EHR Incentive Payment Schedule is shown in Table 1.4
To date, 357,744 Medicare-eligible professionals, 186,147 Medicaid-eligible professionals, and 4847 hospitals have registered for EHR incentive payments.5 The majority of providers and hospitals registered in the first 2 years of the program (2011 and 2012). According to CMS, eligible providers and hospitals have received approximately $21 billion in incentive payments to date: $19.5 billion for Stage 1 and $1.5 billion for Stage 2.5 Of the Stage 1 payments, approximately $7.8 billion has been paid to providers and $11.7 billion to hospitals. For Stage 2 payments, approximately $370 million has been paid to providers and $1.1 billion to hospitals.5
The Medicare EHR Incentive Program began with incentive bonuses but will shift to noncompliance penalties in the coming years. Incentive payments started in 2011 and will continue through 2016. The last year for eligible professionals and hospitals to begin participation and receive an incentive payment, however, was 2014. To receive the maximum incentive payment, eligible professionals must have initiated their participation by 2012. To qualify for incentive payments, eligible professionals must successfully demonstrate meaningful use for each year of participation in the program.3,4
Beginning in 2015, eligible professionals who do not successfully demonstrate meaningful use will be subject to penalties. The payment reduction begins at 1% and increases each year that an eligible professional does not demonstrate meaningful use, to a maximum of 5%.4
There are some important differences between the Medicare and Medicaid EHR Incentive Programs. The Medicaid EHR Incentive Program is administered voluntarily by states and territories, and will pay incentives through 2021. Eligible professionals can participate for 6 years, and the participation years do not have to be consecutive. The last year that an eligible professional can begin his or her participation is 2016. Incentive payments for eligible professionals are substantial; qualifying eligible professionals can earn up to $63,750 in bonuses over 6 years.4
Those eligible professionals who qualify for both the Medicare and Medicaid EHR Incentive Programs, however, must choose the program in which they wish to participate. Medicaid-eligible professionals who also treat Medicare patients will have a payment adjustment to Medicare reimbursements beginning in 2015 if they do not successfully demonstrate meaningful use.4
Differences in the ways in which eligible professionals are defined for Medicare and Medicaid EHR Incentive Programs are shown in Table 2.3
Medicare-eligible hospitals include: (1) “subsection (d) hospitals,” which are general, acute-care, short-term facilities that are paid under the hospital inpatient prospective payment system; (2) critical access hospitals; and (3) Medicare Advantage hospitals.3,6
A hospital is dually eligible for the Medicare and Medicaid EHR Incentive Programs if it is a subsection (d) hospital in the 50 United States or the District of Columbia, or a critical access hospital that meets certain prespecified criteria, including the requirement that at least 10% of its patient volume is derived from those with active Medicaid coverage.3
Modified Objectives for 2015 through 2017
In April 2015, CMS presented its goals for 2015 through 2017, which included modification of the existing rules for Stage 2, as well as its vision for Stage 3 Meaningful Use. During the public comment period for the proposed rules, CMS received a large amount of feedback contending that the current framework for Meaningful Use was too complex and burdensome for medical practices. In response, the agency signaled its intention to simplify the rules and create a structure that was more sustainable for future achievement.7,8 In October 2015, CMS released a Final Rule pertaining to Stage 3, as well as modifications to Meaningful Use from 2015 through 2017.9
In recognition of the issues raised during the public comment period, CMS revised the existing rules in an effort to ease the reporting burden and support health information exchange. According to CMS, the updated regulations will8:
- Allow providers to select measures that are used in their practices and report progress that is most meaningful to their practice
- Give providers and state Medicaid agencies additional time, until January 1, 2018, to comply with the new requirements and prepare for the next set of system improvements
- Support the exchange of health information and a more useful interoperable infrastructure for information exchange between providers and patients.
The updated rules also provide technology developers with more time to create the infrastructure required to enhance ease of use, and align with new models of care and access to data by consumers.8
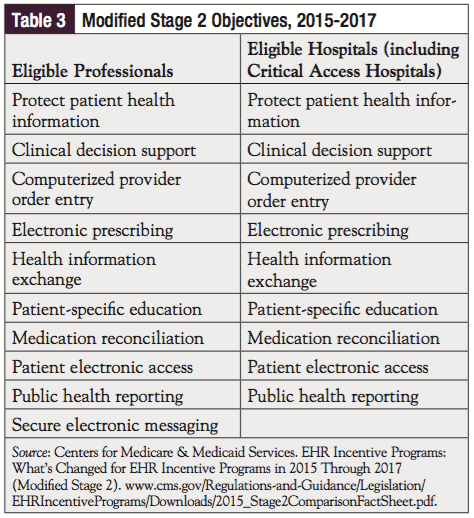
As part of the program enhancements unveiled in the Final Rule, all providers are now required to meet a single set of objectives and measures. These changes remove the menu and core structure of Stages 1 and 2, decrease the overall number of objectives to which a provider must attest, and reduce the reporting burden on measures with which providers have already demonstrated near-universal compliance. As shown in Table 3, of the 10 modified Stage 2 objectives, 9 are the same for both providers and hospitals; eligible professionals are also expected to comply with the secure electronic messaging objective.10
The changes in EHR Incentive Programs took effect on October 6, 2015, for all eligible professionals and eligible hospitals.10 It is important to note that there are several alternate exclusions and specifications for certain measures in 2015 and 2016. CMS has recognized that some providers may not be able to comply with these measures, because they require the implementation of certified EHR technology beyond the functions required for Stage 1. As a result, their compliance thresholds may be lower. A complete listing of alternative exclusions and specifications can be accessed at the following CMS website: www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2015_Stage2ComparisonFactSheet.pdf.10
Beginning with reporting for 2015, the Final Rule has adopted flexible reporting periods that are aligned with other quality initiatives in an effort to reduce the administrative burden for practices and hospitals. Under the revised rules, the EHR reporting period is defined as any continuous 90-day period within the calendar year, rather than the fiscal year. According to CMS, maintaining the 90-day reporting period for new participants in 2016 and 2017 will assist these participants in demonstrating meaningful use in their first year of participation. In addition, providing the 90-day reporting period for new Stage 3 participants in 2017 will help promote flexibility.7,10
All providers are required to use EHR technology certified to the 2014 edition for reporting periods during 2015, 2016, and 2017. If they elect to do so, providers may upgrade early to EHR technology certified to the 2015 edition during this period of time.10
Meaningful Use Stage 3 Criteria
Under the Final Rule, the EHR Incentive Program changes will extend to Stage 3 upon their implementation beginning in 2017. Similar to the enhancements for Stage 2, objectives and measures for Stage 3 include increased thresholds, advanced use of health information exchange functionality, and an overall focus on continuous quality improvement.7,8
For Stage 3 of the EHR Incentive Programs in 2017 and subsequent years, key provisions include the following8:
- A total of 8 core objectives for eligible professionals, eligible hospitals, and critical access hospitals. Health information technology interoperability is a major focus of Stage 3, with more than 60% of the proposed measures requiring interoperability—up from 33% in Stage 2
- Public health reporting is required, with flexible options for measure selection
- Reporting of clinical quality measures, aligned with CMS quality reporting programs
- Measures that enhance the use of application program interfaces, which enable the development of new functionalities to connect systems and provide increased data access for patients.
Stage 3 Implementation
Despite requests to delay Stage 3 implementation, the time line contained in the Final Rule is essentially unchanged compared with the proposed rules.11 Participating hospitals and providers will have the option to report according to Stage 3 criteria in 2017. Providers who elect to begin Stage 3 will have a 90-day reporting period that must fall within the 2017 calendar year. Stage 3 reporting will become a requirement in 2018, regardless of prior participation/stage of meaningful use.7,8
A number of physicians, health information technology professionals, and other healthcare stakeholders have taken issue with the Final Rule as it pertains to Stage 3 implementation. Some of the performance thresholds related to secure patient messaging, integration of patient-generated health data, summary of care requirements, and medication reconciliation are not viewed as realistic, given the fact that fewer than 20% of providers have satisfied the requirements for Stage 2.11
As a result, most providers and hospitals have a great deal of work ahead of them—in terms of health information technology infrastructure, process and workflow improvements, and documentation capacity—to meet the current Meaningful Use certification requirements.12
How Does Meaningful Use Impact Oncology Providers?
The Meaningful Use legislation contains several provisions that pertain to oncology providers.
Oncology-Specific Clinical Quality Measures
One of the Meaningful Use objectives relates to performance improvement on several high-priority medical conditions, including cancer. To that end, beginning in 2014, eligible professionals and hospitals were required to implement 5 clinical decision support interventions related to 4 or more clinical quality measures. As shown in Table 4, there are a total of 64 clinical quality measures to choose from, 7 of which are oncology-specific. Participants only need to demonstrate the ability to report on these measures; they are not required to meet any preset threshold at this time.9,13
Cancer Registry Reporting for Eligible Professionals
The Centers for Disease Control and Prevention maintains that certified EHR technology can improve the cancer reporting and surveillance process.14 As a result, public health reporting was cited as one of the core Meaningful Use program objectives for 2015 and beyond. The program encourages providers to actively submit data to a public health agency, including state cancer registries, immunization registries, or other disease-specific registries.13
Since cancer registry reporting is already routine practice for hospitals providing cancer care, the Final Rule was updated to incorporate cancer case reporting for eligible professionals only. According to the legislation, eligible professionals are permitted to report applicable cancer cases under the Specialized Registry Reporting measure. Successful reporting with respect to this measure will count toward Meaningful Use attestation for eligible oncology professionals.9
Participation in the Oncology Care Model
In addition to the other oncology-specific requirements promulgated by the Final Rule, CMS has tied Oncology Care Model participation to Meaningful Use proficiency, by including attestation as a requirement for participating in the agency’s new Oncology Care Model.15
Prior to initiating active engagement in the Oncology Care Model, participating practices are required to demonstrate their intent to meaningfully use EHR technology. By the end of the first performance year, eligible professionals in a participating practice must attest to Stage 1 of Meaningful Use, with the intention of attesting to Stage 2 of Meaningful Use by the end of the third performance year.15
References
1. Centers for Medicare & Medicaid Services. Electronic Health Records (EHR) Incentive Programs. www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms. Accessed November 22, 2015.
2. HealthIT.gov. Meaningful Use Definitions and Objectives. www.healthit.gov/providers-professionals/meaningful-use-definition-objectives. Accessed November 22, 2015.
3. HealthIT.gov. EHR Incentive Programs. www.healthit.gov/providers-professionals/ehr-incentive-programs. Accessed November 23, 2015.
4. Centers for Medicare & Medicaid Services. Medicare and Medicaid EHR Incentive Program Basics. www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Basics.html. Accessed November 23, 2015.
5. Centers for Medicare & Medicaid Services. EHR Incentive Program summary report, September 2015. www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/September2015_SummaryReport.pdf. Accessed November 23, 2015.
6. American College of Emergency Physicians. Medicare Hospital Readmission Reduction Program FAQ. www.acep.org/Physician-Resources/Practice-Resources/Administration/Financial-Issues-/-Reimbursement/Medicare-s-Hospital-Readmission-Reduction-Program-FAQ/. Accessed November 28, 2015.
7. Healthcare IT News. CMS lays out vision for Stage 3 meaningful use. www.healthcareitnews.com/news/cms-lays-out-vision-stage-3-meaningful-use?single-page=true. Accessed November 24, 2015.
8. Centers for Medicare & Medicaid Services. CMS Fact Sheet: EHR Incentive Programs in 2015 and Beyond. www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-10-06-2.html. Accessed November 24, 2015.
9. Federal Register. Medicare and Medicaid Programs; Electronic Health Record Incentive Program-Stage 3 and Modifications to Meaningful Use in 2015 Through 2017; Final Rule. Vol. 80, No. 200, October 16, 2015. www.federalregister.gov/articles/2015/10/16/2015-25595/medicare-and-medicaid-programs-electronic-health-record-incentive-program-stage-3-and-modifications. Accessed December 10, 2015.
10. Centers for Medicare & Medicaid Services. EHR Incentive Programs: What’s Changed for EHR Incentive Programs in 2015 Through 2017 (Modified Stage 2). www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2015_Stage2ComparisonFactSheet.pdf. Accessed November 24, 2015.
11. Practice Fusion (blog). Meaningful Use Stage 3 – 2015 Certification final rules released. www.practicefusion.com/blog/meaningful-use-stage-3/. Accessed November 25, 2015.
12. Fierce EMR. Stage 3 Meaningful Use rules ambitious but burdensome, providers say. www.fierceemr.com/story/stage-3-meaningful-use-rules-ambitious-burdensome-providers-say/2015-03-23. Accessed November 27, 2015.
13. American Society of Clinical Oncology. The Meaningful Use Incentives – Stage 2: A Guide to the Objectives and Measures. www.asco.org/sites/www.asco.org/files/asco_summary_of_meaningful_use_stage_2_final_5.22.13.pdf. Accessed December 16, 2015.
14. Centers for Disease Control and Prevention. Meaningful Use of Electronic Health Records. www.cdc.gov/cancer/npcr/meaningful_use.htm. Accessed December 16, 2015.
15. FierceEMR. CMS Oncology Care Model requires Meaningful Use participation. www.fierceemr.com/story/cms-oncology-care-model-requires-meaningful-use-participation/2015-02-16. Accessed December 16, 2015.